Hidden Mechanisms of Drug Resistance in Patients with Blast-phase Chronic Myeloid Leukemia Discovered
Collaborative research with Professor Dong-Wook Kim’s team at Uijeongbu Eulji Medical Center discovers mechanisms of resistance to targeted agents
Securing source technology for FLT3-TAZ signal transmission system control
BCR::ABL1+FLT3 inhibitor combination overcomes resistance and identifies a potential for a cure
Professor Hyun Woo Park of the Department of Biochemistry at Yonsei University and his team have identified a novel molecular mechanism by which chronic myeloid leukemia (CML) cells acquire drug resistance to BCR::ABL1-targeted agents, suggesting a new treatment for patients with blast-phase chronic myeloid leukemia (BP-CML), an incurable disease.
The study, which was conducted over three years in collaboration with Professor Dong-Wook Kim’s team of the Hematologic Tumor Medicine Department at the Uijeongbu Eulji Medical Center, was published online on November 6, 2023, in “Molecular Cancer (IF 37.3),” a leading journal in the field of cancer biology.
The causative gene for chronic myeloid leukemia is the BCR::ABL1 gene, which results from translocations on chromosomes 9 and 21, and is divided into a chronic phase (CP) and a blast phase (BP), depending on the severity of the disease. Imatinib (Gleevec), a first-generation BCR::ABL1-targeted agent approved by the U.S. FDA in 2001, has been associated with the progression to the blast phase and the acquisition of drug resistance in some patients when taken continuously. This has led to the development of second- and third-generation targeted agents such as nilotinib, dasatinib, and ponatinib; however, patients still die from either the progression to the blast phase or drug resistance.
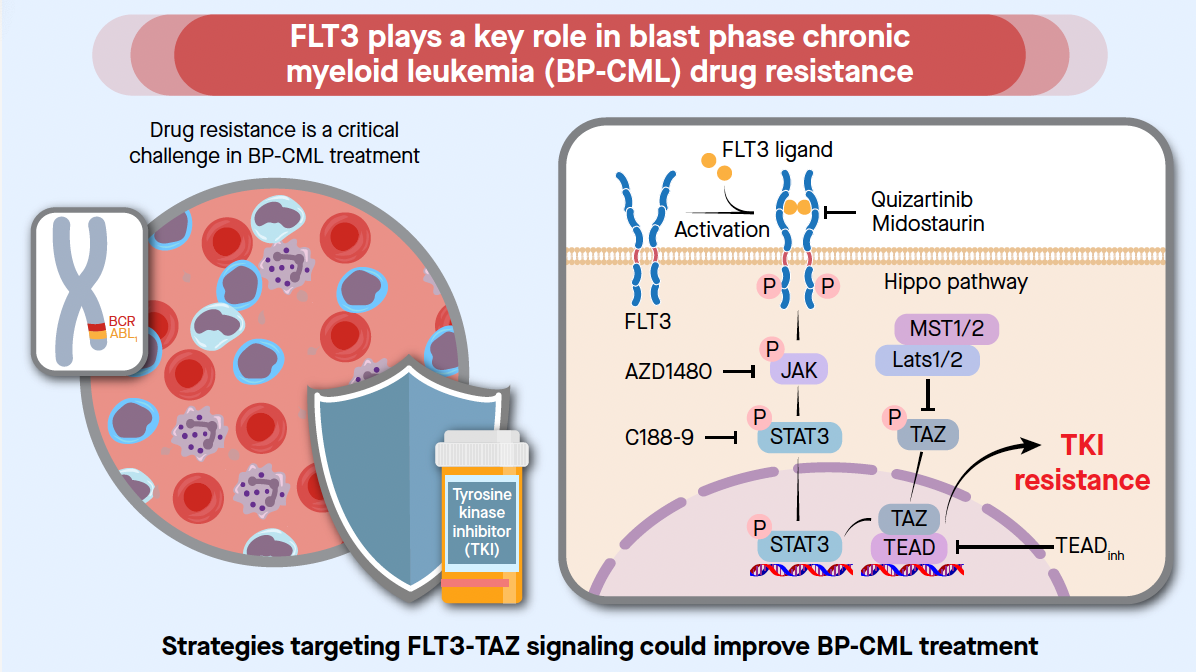
Cell proliferation in patients with chronic myeloid leukemia (CML), who progressed to a blast phase after failing treatment with targeted agents, resembled acute myeloid leukemia (AML). Based on this, the team examined the expression of genes associated with acute myeloid leukemia, such as FLT3. In general, collecting samples from patients in the blast phase with a poor prognosis is challenging, making research utilizing these samples extremely difficult. However, experiments were conducted by selecting a cohort with differentiated characteristics using human derivative samples and clinical information collected during the chronic and blast phases of the disease by the Hematologic Tumor Medicine Department at the Uijeongbu Eulji Medical Center.
First, the comparison of FLT3 membrane receptor expression in chronic and blast-phase myeloid leukemia patients revealed that, surprisingly, the FLT3 membrane receptor was increased in more than half of the blast-phase patients, whereas it was not expressed at all in the chronic phase.
This led to the first discovery of the potential use of FLT3 inhibitors, which have recently begun to be used to treat patients with acute myeloid leukemia as a treatment for drug.
In fact, the team found in samples from patients with hematological malignancies and animal studies that the combination of a newly designed combination therapy — a BCR::ABL1 inhibitor and an FLT3 inhibitor — increased the drug sensitivity of human leukemia cells, allowing them to overcome the drug resistance of all currently known tyrosine kinase inhibitors (TKIs, targeted anti-cancer drugs for chronic myeloid leukemia). In particular, using FLT3 inhibitors in the chronic phase was found to help prevent future drug resistance.
Professor Park’s team also noted that ponatinib, a third-generation BCR::ABL1 inhibitor, was a compound that simultaneously targeted FLT3 as well as BCR::ABL1. Surprisingly, ponatinib as a single agent was as effective as the combination of FLT3 inhibitors with the previously used BCR::ABL1 inhibitors — including imatinib, radotinib, nilotinib, and dasatinib — in suppressing drug resistance.
As a result, it was revealed for the first time that ponatinib, used as a treatment drug for patients with chronic myeloid leukemia in the blast phase, could be used for treatment or prevention by overcoming resistance to targeted agents caused by FLT3. In addition, future drugs being developed as FLT3 inhibitors are expected to be tested in conjunction with BCR::ABL1 inhibitors for their ability to suppress drug resistance, leading to a new phase of research in this field.
The team further analyzed the molecular mechanisms of drug resistance through FLT3. As a result, the FLT3 membrane receptor was found to be expressed in the blast phase of chronic myeloid leukemia, activating the downstream signaling system of "FLT3-JAK-pSTAT3-TAZ-TEAD-CD36." TAZ and TEAD are transcription factors involved in adherent-to-suspension transition (AST), first identified by the team, and are not expressed at all in normal blood cells. They are, however, expressed in human leukemia cells, leading to a suspension-to-adherent transformation, treatment resistance to existing drugs, and metastasis. This is the first discovery that TAZ-TEAD inhibitors — which are currently in active development for the treatment of solid tumors — may also be applicable to the treatment of patients with hematologic malignancies.
Furthermore, by identifying the CD36 fatty acid transporter as a novel gene target of the TEAD transcription factor, this study demonstrated that the combination of a CD36 inhibitor and a low-fat diet could enhance the therapeutic effectiveness for patients with blast-phase chronic myeloid leukemia.
Based on these findings, the team successfully conducted translational research and industrialization, including domestic and international patent applications, registrations, and technology transfer, and secured the original technology for controlling the FLT3-TAZ signaling system to suppress drug resistance in patients with chronic myeloid leukemia.
"This study is the first in the world to identify a novel anti-cancer treatment and diagnostic strategy using FLT3 for patients with blast-phase chronic myeloid leukemia with a very poor prognosis," said Yonsei University Professor Park. "It will contribute to the development of new bio-diagnostic markers and next-generation therapeutics for hematological malignancies using the gene and protein sequences of FLT3."
"Many patients with chronic myeloid leukemia, who must receive chemotherapy for life, develop resistance to the agents or rapidly transition to the blast phase of the disease, making it difficult to treat," said Professor Kim at the Uijeongbu Eulji Medical Center. "This study suggests a new treatment to prevent resistance, bringing us closer to 'curing' leukemia."
The research was supported by the Convergence Research and Development Project for Scientific Challenges of the Ministry of Science and ICT and the National Research Foundation (NRF) of Korea, the Mid-Career Researcher Support Project, the Seo Kyung-bae Science Foundation (Yonsei University), and the Next Generation Applied Omics Project for Biomedical Technology Development (Eulji University).
Find out more:
Title of original article: Targeting FLT3-TAZ Signaling to Suppress Drug Resistance in Blast Phase Chronic Myeloid Leukemia
DOI: https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01837-4
Journal: Molecular Cancer
Contact corresponding author: Prof. Hyun Woo Park (hwp003@yonsei.ac.kr)
Recommended Articles
Professor Byeong-Su Kim
New study demonstrates that “deformable” electronics are not a stretch
Professor Yeonjin Yi